Head Trauma, Stroke and Parkinson's Disease:
Head Trauma:
Brain trauma from concussions or repeated hits to the head can increase the risk for Parkinson's later in life. Muhammad Ali is probably the most famous celebrity who's years of boxing and blows to the head, resulted in Parkinson's disease. A study conducted by Paul K. Crane, M.D., M.P.H., at the University of Washington concluded that brain trauma was associated with:- the development of Lewy bodies resulting from neuron death by alpha-synuclein protein, the underlying cause of Parkinson's disease.
- microscopic strokes in the brain called "Microinfarcts"
- Traumatic Brain Injury (TBI) with Loss Of Consciousness (LOC) longer than an hour was associated with 3 1/2 times increased risk of developing Parkinson's disease. It was equaly important to note that the vast majority of people who experience head injury will not develop Parkinson’s disease.
This study included 7,130 people with head injury data.
A study of more than 300,000 US veterans of which half were diagnosed with mild traumatic brain injury (TBI) due to explosions, found that more than 50% of them were at increased risk of developing Parkinson's disease even after adjusting for age and other demographics. Those more severely injured were associated with an even higher risk.
Reference Mild TBI and risk of Parkinson disease: A Chronic Effects of Neurotrauma Consortium Study
Stroke and TIA:
Parkinsonism is any condition which causes any of the movement disorders associated with Parkinson's Disease such as tremors, slow movement, impaired speech or stiff muscle movement. Parkinson's Disease is a single and a prevalent cause of Parkinsonism, but not the only cause. There are two forms of a stroke, an ischemic stroke which is caused by blood vessel blockage and hemorrhagic strokes caused by internal bleeding. About 87% of strokes are ischemic, the rest being hemorrhagic. Strokes including "small vessel strokes" can cause Vascular (Multi-Infarct) Parkinsonism by directly affecting the substantia nigra or the basal ganglia regions of the brain. Vascular Parkinsonism often involves the lower part of the body more than the upper part of the body and typically develops symptoms of parkinsonism on the opposite side of the body from the area of the brain affected. The blood vessel blockage is typically casued by:
- thickening of the blood vessel wall due to high blood pressure also know as "lipohyalinosis"
- fatty deposits on the arterial walls resulting in hardening of the arteries and known as "atherosclerosis"
- blood clot from the inner lining of another blood vessel or from the heart which lodges in a blood vessel in the brain in a process known as "embolization"
The atherosclerotic blockage and lesions are composed of cellular material, blood vessle muscle, macrophages, lipid particles, cholesterol crystal, calcification, fibrous overgrowths and connective tissue.
Vascular health can be improved with Omega-3 and Niacin (vitamin B3) supplements. Studies have shown that the combination produced additive effects. Niacin reduces serum triglyceride (fat) levels and LDL (bad cholesterol) while raising HDL (good cholesterol). Omega-3 also reduces serum triglyceride levels and serves as an anti-coagulant. Omega-3 food sources include fish (choose low mercury, short lived, low on the food chain varieties like sardines, salmon, tilapia and avoid tuna, swordfish, shark) and avocados.
It has also been shown that vitamin D3 and K can improve vascular health. Vitamin D3 in combination with vitamin K can help with the absorption of calcium in the gut and remove calcium from the vascular compartment for storage in the bones, helping prevent osteoporosis and lowering the chance of stroke.
A statin like Lipitor can be added to lower cholesterol with a doctor's prescription. Low dose aspirin or prescription blood thinner can be added to avoid the coagulation of platelets which can block blood vessels. Anti-coagulants can only be used for ischemic strokes and will only worsen the condition of a hemorrhagic stroke. Also note that while aspirin is an over-the-counter medication, it can cause internal bleeding. Its misuse is not without consequences. In cases of extreme atherosclerosis, chelation with EDTA (specifically the NaMgEDTA variant which is preferred for targeting calcium and treating vascular disease ref) can clear out calcium deposits and plaque. Refer to the National Institute of Health (NIH) Trial to Assess Chelation Therapy (TACT) studies (ref). All medications should be taken under the guidance of a health professional.
References:- Effects of prescription niacin and omega-3 fatty acids on lipids and vascular function in metabolic syndrome: a randomized controlled trial (2012)
- Niacin in Cardiovascular Disease: Recent Preclinical and Clinical Developments (2012)
- Atherosclerosis: from biology to pharmacological treatment (2012 meta study)
- Comparison of chelating agents DMPS, DMSA and EDTA for the diagnosis and treatment of chronic metal exposure (2014: British Journal of Medicine and Medical Research)
Stroke Treatments:
Strokes can cause movement disorders which mimic Parkinson's and affect motor neurons but are treated as a stroke. Therapies include pharmalogical, electrical and physical therapies.
Brief list of stroke rehabilitation therapies:- Pharmalogical:
- Selective Serotonin Reuptake Inhibitors (SSRI): increases the extracellular levels of neurotransmitter serotonin and improves motor rehabilitation. Enhancement of synaptic plasticity, neurogenesis, synaptogenesis, and dendritic remodeling. eg fluoxetine
- Noradrenaline Reuptake Inhibitors (NARI): increases the extracellular levels of neurotransmitter noradrenaline and has neurorestorative properties, Enhancement of synaptic plasticity, neurogenesis, synaptogenesis, and dendritic remodeling. eg reboxetine
- Electrical:
- Repetitive Transcranial Magnetic Stimulation (rTMS): is a painless, non-invasive technique using a rapidly changing magnetic field initiated by a brief high intensity electric current, passes through a coil over the scalp.
- Transcranial Direct Current Stimulation (tDCS): is a noninvasive application of weak electrical current to brain tissue which reduces interhemispheric imbalance and improves brain plasticity.
- Physical Therapy:
- Robot-assisted therapy: a re-programmable, multi-functional manipulator designed to move limbs through variable programmed motions (low effectivity)
- Virtual Reality: computerized techniques allow subjects to interact with a virtual environment (low effectivity)
- Neurologic Music Therapy (NMT): therapeutic application of music with rhythmic auditory cueing of movement execution as well as motivational aspects (low effectivity)
- Mirror Therapy: View body motion by way of a mirror to activate motor neurons via their mirror neurons
- Modified Constraint-Induced Movement Therapy (mCIMT): involves the restraint of the individual’s less impaired upper extremity with the use of a safety mitt. The less affected upper extremity is placed in constraint with the expectation that the patient will try and use the more affected upper extremity for everyday activities.
- Muscle strengthening exercises
- Rehabilitation of Motor Function after Stroke: A Multiple Systematic Review Focused on Techniques to Stimulate Upper Extremity Recovery (2016)
DOI: 10.3389/fnhum.2016.00442 - Enhancing endogenous capacity to repair a stroke-damaged brain: An evolving field for stroke research (2018) extensive review
DOI: 10.1016/j.pneurobio.2018.01.004

MRI:

Magnetic Resonance Imaging (MRI) systems will have the capability to take a high resolution scan of the brain, revealing areas affected by stroke. MRIs can produce higher resolution images than Computed Tomography (CT) scans.
Viewing MRI images:
One can obtain a CD or DVD of the MRI images or datasets which can be viewed with viewing software included or with the Java based (runs on MS/Windows, Apple Mac, Linux) open source software Medical Image Processing, Analysis, and Visualization (MIPAV) developed by the US National Institutes of Health (NIH) Center for Information Technology (CIT).
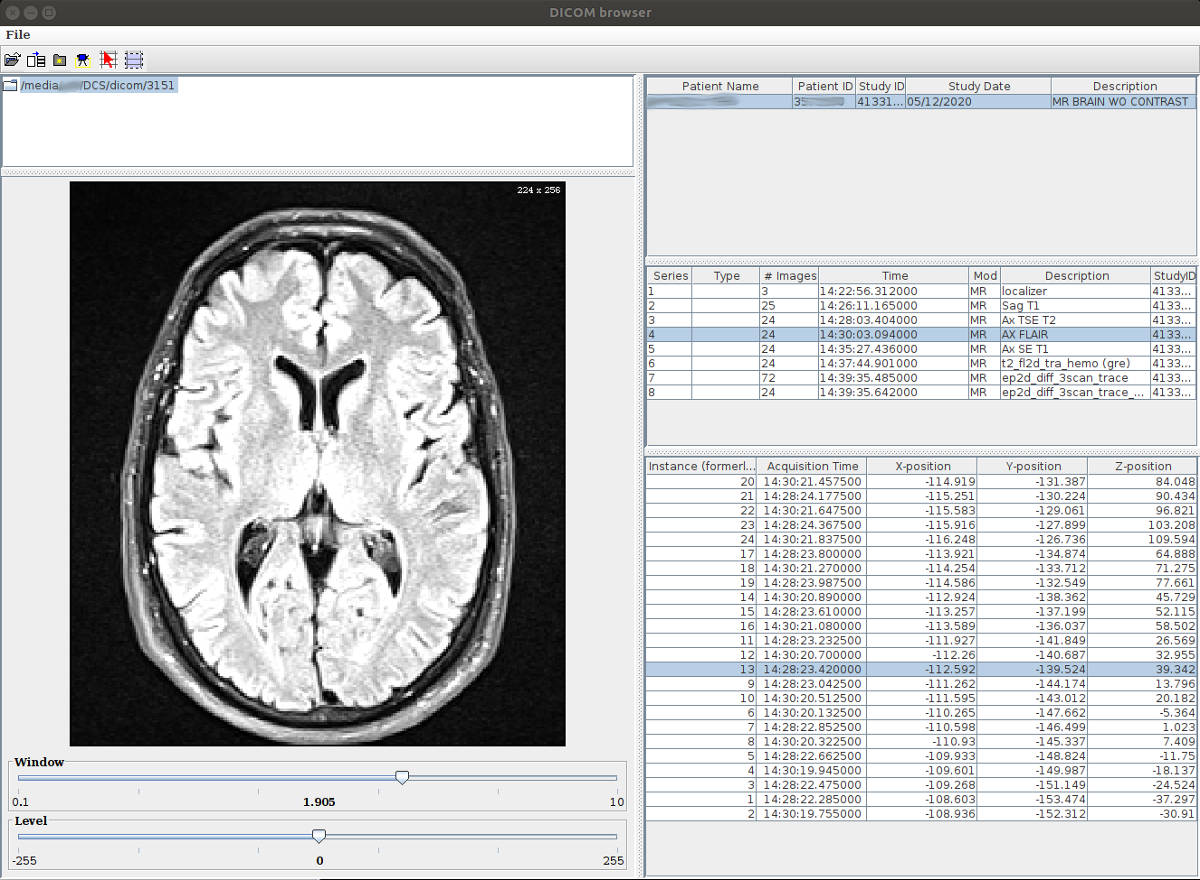
MIPAV: point it to the top image directory on the DVD and select the "Parse Directory" icon, then just click on the various images to view them.